Possibility of COVID-19 Illness After Vaccination
November 12, 2021COVID-19 vaccines are effective at preventing infection, serious illness, and death. Most people who get COVID-19 are unvaccinated. However, since vaccines are not 100% effective at preventing infection, some people who are fully vaccinated will still get COVID-19.
An infection of a fully vaccinated person is referred to as a “vaccine breakthrough infection”.
Key Points
- COVID-19 vaccines protect everyone ages 5 years and older from getting infected and severely ill, and significantly reduce the likelihood of hospitalization and death.
- Getting vaccinated is the best way to slow the spread of COVID-19 and to prevent infection by Delta or other variants.
- A vaccine breakthrough infection happens when a fully vaccinated person gets infected with COVID-19. People with vaccine breakthrough infections may spread COVID-19 to others.
- Even if you are fully vaccinated, if you live in an area with substantial or high transmission of COVID-19, you – as well as your family and community – will be better protected if you wear a mask when you are in indoor public places.
- People who are immunocompromised may not always build adequate levels of protection after an initial 2-dose primary mRNA COVID-19 vaccine series. They should continue to take all precautions recommended for unvaccinated people, until advised otherwise by their healthcare professional. Further, CDC recommends that moderately to severely immunocompromised people can receive an additional primary dose of the vaccine.
What We Know About Vaccine Breakthrough Infections
- Vaccine breakthrough infections are expected. COVID-19 vaccines are effective at preventing most infections. However, like other vaccines, they are not 100% effective.
- Fully vaccinated people with a vaccine breakthrough infection are less likely to develop serious illness than those who are unvaccinated and get COVID-19.
- Even when fully vaccinated people develop symptoms, they tend to be less severe symptoms than in unvaccinated people. This means they are much less likely to be hospitalized or die than people who are not vaccinated.
- People who get vaccine breakthrough infections can be contagious.
CDC is collecting data on vaccine breakthrough infections and is closely monitoring the safety and effectiveness of all Food and Drug Administration (FDA) approved and authorized COVID-19 vaccines.
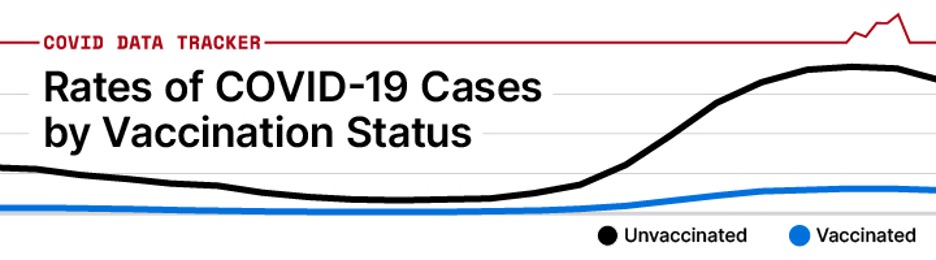
Because vaccines are not 100% effective, as the number of people who are fully vaccinated goes up, the number of vaccine breakthrough infections will also increase. However, the risk of infection remains much higher for unvaccinated than vaccinated people.
The latest data on rates of COVID-19 cases, hospitalizations, and deaths by vaccination status are available from the CDC COVID Data Tracker.
Vaccine Breakthrough and Variants
CDC continues to actively monitor vaccine safety and effectiveness against new and emerging variants for all FDA-authorized COVID-19 vaccines. Research shows that the FDA-authorized vaccines offer protection against severe disease, hospitalization, and death against currently circulating variants in the United States. However, some people who are fully vaccinated will get COVID-19.
The Delta variant is more contagious than previous variants of the virus that causes COVID-19. However, studies so far indicate that the vaccines used in the United States work well against the Delta variant, particularly in preventing severe disease and hospitalization.
Overall, if there are more COVID-19 infections, there will be more vaccine breakthrough infections. However, the risk of infection, hospitalization, and death is much lower in vaccinated compared to unvaccinated people. Therefore, everyone ages 5 years and older should get vaccinated to protect themselves and those around them, including family members who are not able to be vaccinated from severe disease and death.
How CDC Monitors Breakthrough Infections
CDC has multiple surveillance systems and ongoing research studies to monitor the performance of vaccines in preventing infection, disease, hospitalization, and death. CDC also collects data on vaccine breakthrough infections through outbreak investigations.
About COVID-NET
One important system that CDC uses to track vaccine breakthrough infections is COVID-NET (The Coronavirus Disease 2019 [COVID-19]-Associated Hospitalization Surveillance Network). This system provides the most complete data on vaccine breakthroughs in the general population. COVID-NET is a population-based surveillance system that collects reports of lab-confirmed COVID-19 related hospitalizations in 99 countries, in 14 states.
COVID-NET covers approximately 10% of the US population. One recent COVID-NET publication assessed the effectiveness of COVID-19 vaccines in preventing hospitalization among adults 65 years and older. This system provides complete data on vaccine breakthrough hospitalizations in the general population.
Examples of CDC’s Systems for Monitoring:
| Outcome Monitored | Population Monitored | Monitoring System |
| Infection | Long-term care facility residents | NHSN |
| Infection and symptomatic illness | Healthcare providers and frontline workers | HEROES/RECOVER |
| Hospitalizations and deaths | Hospitalized adults | IVY |
| Hospitalizations and deaths | Hospitalized people (all ages) | COVID-NET |
| Urgent care, emergency care, hospitalization, and deaths | Urgent Care, emergency departments, and hospitalized people (all ages) | VISION |
Voluntary Reporting by State Health Departments
When the United States began widespread COVID-19 vaccinations, CDC put in place a system where state health departments could report COVID-19 vaccine breakthrough infections to CDC.
On May 1, 2021, after collecting data on thousands of vaccine breakthrough infections, CDC changed the focus of how it uses data from this reporting system.
- One of the strengths of this system is collecting data on severe cases of COVID-19 vaccine breakthrough infections since it is likely that most of these types of vaccine breakthrough cases seek medical care and are diagnosed and reported as a COVID-19 case.
- Persons with asymptomatic or mild cases of vaccine breakthrough infections may not seek testing or medical care and thus these types of vaccine breakthrough cases may be underrepresented in this system. For this reason, CDC relies on a variety of additional surveillance approaches to ensure that it is collecting information on all types of vaccine breakthrough cases.
- CDC continues to monitor data on all cases reported by the state health department as vaccine breakthrough cases. Currently, 49 states have reported at least one vaccine breakthrough infection to this system.